ERCP
A supple flexible tube fitted with high definition camera & light is passed through the anus to visualize the large intestine ( colon ) & rectum.
ERCP
A supple flexible tube fitted with High Definition camera & light is passed through the anus to visualize the large intestine ( Colon ) & rectum.
ERCP stands for Endoscopic Retrograde Cholangiopancreatography. It is a medical procedure that combines endoscopy and x-ray imaging to diagnose and treat conditions related to the bile ducts, pancreas, and liver. During an ERCP, a flexible tube called an endoscope is inserted through the mouth, down the esophagus and stomach, and into the duodenum (the first part of the small intestine). The endoscope has a light and a camera on the tip, allowing the doctor to visualize the bile ducts and pancreas.
1,11,1000+ CASES HANDLED
3 HI-TECH ENDOSCOPY DEVICES
5+ SPECIALIST GI ENDOSCOPIST
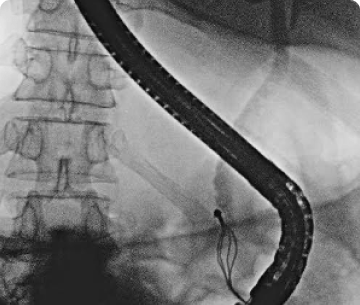
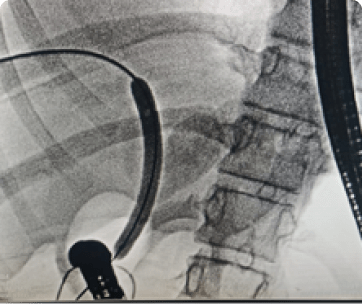
The procedure is done under short general anesthesia to reduce patients’ discomfort and pain experienced during the procedure. A Side viewing scope (endoscope with a camera on the side of the tip of the endoscope) visualizes the side walls of the duodenum (1st part of the small intestine) where the papilla (opening of bile duct and pancreatic duct) is located. The bile or pancreatic duct is selectively cannulated (thin, flexible wire is passed over, and which catheter is pushed). A radiopaque dye is then injected through the cannula to visualize the duct anatomy, including stones or strictures (narrowing of the duct) or leaks on fluoroscopy (X-ray). The stones are removed, strictures are dilated with the balloon, and a stent (plastic tube) is placed in the selected duct for adequate drainage.
Biliary:
Bile duct stones
Bile duct strictures
Bile duct leaks (After gall bladder drainage)
Biliary pancreatitis
Obstructive jaundice due to pancreatic cancers
Pancreatic:
Pancreatic stones
Pancreas divisum (congenital abnormality in the pancreatic duct)
Pancreatic leaks with ascites, pseudocyst, pleural effusion
Pancreatic strictures
The patient should be fasting for 6-8 hours before the procedure
Cardiologist or physician fitness is taken
IV antibiotics are given
The patient is started on saline
Antiplatelets or anticoagulants (blood thinners) should be stopped as per physician or cardiologist advice for 2-7 days before the procedure.
The patient may experience bloating, mild pain, or vomiting post-procedure; other complications are:
Pancreatitis (pancreas edema)
Bleeding
Perforation (hole in the intestine)
The procedure is done under short general anesthesia to reduce patients’ discomfort and pain experienced during the procedure. A Side viewing scope (endoscope with a camera on the side of the tip of the endoscope) visualizes the side walls of the duodenum (1st part of the small intestine) where the papilla (opening of bile duct and pancreatic duct) is located. The bile or pancreatic duct is selectively cannulated (thin, flexible wire is passed over, and which catheter is pushed). A radiopaque dye is then injected through the cannula to visualize the duct anatomy, including stones or strictures (narrowing of the duct) or leaks on fluoroscopy (X-ray). The stones are removed, strictures are dilated with the balloon, and a stent (plastic tube) is placed in the selected duct for adequate drainage.
Biliary:
Bile duct stones
Bile duct strictures
Bile duct leaks (After gall bladder drainage)
Biliary pancreatitis
Obstructive jaundice due to pancreatic cancers
Pancreatic:
Pancreatic stones
Pancreas divisum (congenital abnormality in the pancreatic duct)
Pancreatic leaks with ascites, pseudocyst, pleural effusion
Pancreatic strictures
The patient should be fasting for 6-8 hours before the procedure
Cardiologist or physician fitness is taken
IV antibiotics are given
The patient is started on saline
Antiplatelets or anticoagulants (blood thinners) should be stopped as per physician or cardiologist advice for 2-7 days before the procedure.
The patient may experience bloating, mild pain, or vomiting post-procedure; other complications are:
Pancreatitis (pancreas edema)
Bleeding
Perforation (hole in the intestine)
PROCEDURES WE CONDUCT
FREQUENTLY ASKED QUESTIONS
FREQUENTLY ASKED QUESTIONS
Don’t wait!!
Get consulted with our GI specialist today
Book your appointment effortlessly.
ANTRANG KNOWLEDGE RESOURCE
ANTRANG KNOWLEDGE RESOURCE
get in touch
We are just a phone call away when you need us!