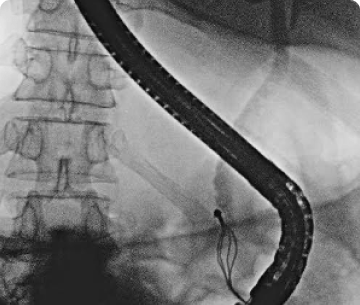
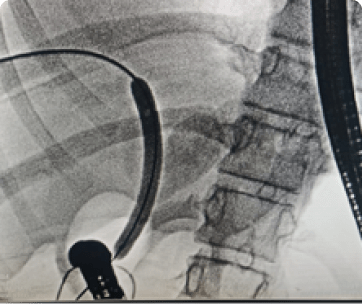
26yr old female presented with cholangitis. She had underwent choledochojejunostomy at 16yrs of age for choledochal cyst. On CT she had developed anastomotic stricture with dilated CHD and IHBR with multiple stones. We attempted a spiral enteroscopy but couldn’t reach the stricture due to acute bend. She underwent PTBD to relive her cholangitis. She was explained regarding Sx hepaticojejunostomy or to get subcutaneous access biliary limb for recurrent stricture dilatation. But patient did not want any surgical intervention, so after detailed counselling and informed consent we did a EUS guided duodenojejunostomy (but placing a 20mm x 10mm Hot Axios stent to create an anastomosis between 1st part of duodenum and the biliary jejunal limb). Pt had no complications post procedure and was started on oral feeds liquids followed by solids 6hrs post procedure and was discharged next day. She was called after 2 weeks, we could reach the strictured choledochojejunostomy site through the duodenojejunstomy stent with a normal gastroscope. PTBD stent was removed. We dilated the stricture up to 8mm with a CRE balloon, and removed multiple stones and put a plastic stent.
Now we have access to the strictured choledochojejunostomy site and can dilate it as and when it’s required and can be done under short GA on OPD basis.
We attempted ERCP and we were successful in placing stent across the cystic cavity from the papilla upto the tail of the pancreas. Presently we have keep the gastrocystostomy stent and the PD stent in Situ and will plan to remove both the stents if the Disconnect pancreatic duct heals ,so that there is no recurrence of the pseudocyst due to persisting pancreatic ductal leak.
Discussion
Rupture of WOPN is a rare condition.WOPN can rupture into the gastrointestinal lumen or in the peritoneal cavity. The rupture of WOPN into the peritoneal cavity is difficult to treat and has dilemmas in management approach. It can leads to high possibilities of infections, pancreatic fistulas and carries high mortality. We present a case series of 8 patients of acute necrotizing pancreatitis with disconnected pancreatic duct syndrome (DPDS) and walled off pancreatic necrosis (WOPN) with spontaneous rupture. Two patients had rupture into the GI tract (1 in the antrum and 1 in 1st part of duodeum). 2 plastic stents were placed through the luminal opening into the pseudocyst cavity to create an internal fistula and later underwent ERCP with pancreatic duct (PD) stenting. 6 patient had a rupture in the perinoteal cavity causing pancreatic peritonitis. Ascitis was aspirated for diagnosis with ascitic amylase ranging from 8945 to 25768 U/L. All patients presented with high grade fever and systemic inflammatory response syndrome (SIRS).
The average size of the WOPN was 8 cms with wall thickness of 4 mm. Surgical gastrocystostomy was not possible. 5 patients underwent endoscopic ultrasound guided gastrocystostomy with lumen opposing metal stent (LAMS) to drain the WOPN and create an internal fistula, followed by ERCP with PD stenting. 3 patients had clear ascitic fluid so were drained by percutaneous pigtail drainage. 2 patients had multiple internal septations in the ascitic fluid, hence were later subjected to a laparotomy with peritoneal lavage and external drain placement. One patient had a complete rupture of the WOPN with no residual collection, hence only PD stent followed by peritoneal lavage was done. All patients were on broad spectrum antibiotics and nasojejunal feeds. None of patients required endoscopic pancreatic necrosectomy. There was no mortality, no external pancreatic fistula and the average hospital stay was 10 days. This is the first case series of 8 patients with partially ruptured WOPN managed successfully.